Bariatric Surgery Frequently Asked Questions – FAQs
Bariatric surgery is an operation that helps you lose weight by making changes to your digestive system.
Laparoscopic Bariatric Surgery
Some types of bariatric surgeries make your stomach smaller, allowing you to eat and drink less at one time and making you feel full sooner. Other bariatric surgeries also change your small intestine—the part of your body that absorbs calories and nutrients from foods and beverages.
Bariatric surgery may be an option if you have severe obesity and have not been able to lose weight or keep from gaining back any weight you lost using other methods such as lifestyle treatment or medications. Bariatric surgery also may be an option if you have serious health problems, such as type 2 diabetes or sleep apnea, related to obesity. Bariatric surgery can improve many of the medical conditions linked to obesity, especially type 2 diabetes.*
Having surgery to lose weight is a serious decision. If you are thinking about having bariatric surgery, you should know what’s involved. Your answers to the following questions may help you decide if surgery is an option for you:
- Have you been unable to lose weight or keep it off using nonsurgical methods such as lifestyle changes or drug treatment?
- Do you understand what the operation involves and its risks and benefits?
- Do you understand how your eating and physical activity patterns will need to change after you have surgery?
- Can you commit to following lifelong healthy eating and physical activity habits, medical follow-up, and the need to take extra vitamins and minerals?
Read More: This content is provided as a service of the The National Institute of Diabetes and Digestive and Kidney Diseases, Health Information Center.
Bariatric procedures are considered major surgery, and you must consider the risks and long-term health benefits. Bariatric surgery may help you reduce or eliminate some diseases such as described in the table below.
Health Problem (Comorbidity) |
Result After Gastric Bypass Surgery |
|---|---|
| • Type 2 Diabetes | – Resolved† in 83.7% of patients. |
| • High Blood Pressure | – Resolved in 67.5% of patients |
| • High Cholesterol | – Improved†† in 94.9% of patients |
| • Obstructive Sleep Apnea | – Resolved in 80.4% of patients |
| • Acid Reflux/GERD | – Resolved in 98% of patients |
| • Depression | – Improved in 47% of patients |
| • Osteoarthritis and Joint Pain | – Resolved in 41% of patients |
| • Stress Urinary Incontinence | – Resolved in 44% of patients |
† In medical terminology, “resolved” is defined as removing all known symptoms and signs of the condition or disease.
†† In medical terminology, “improved” is defined as reducing the known symptoms and signs of the condition or disease.
To read more about the benefits of weight-loss surgery, visit the Weight-control Information Network (WIN) website.
What is the difference between open and laparoscopic surgery?
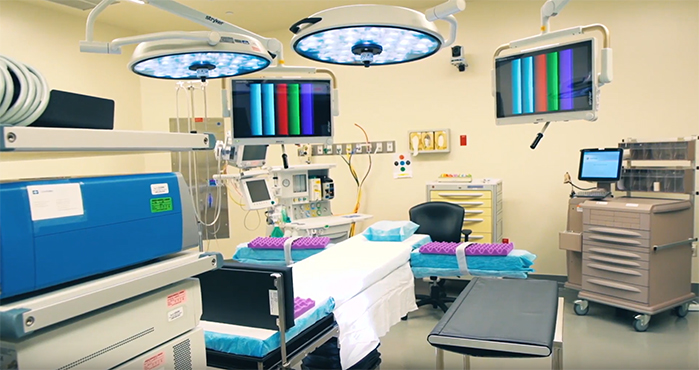
In open bariatric surgery, surgeons make a single, large cut in the abdomen. More often, surgeons now use laparoscopic surgery, in which they make several small cuts and insert thin surgical tools through the cuts. Surgeons also insert a small scope attached to a camera that projects images onto a video monitor.
Laparoscopic Surgery Suite at First Baptist Medical Center
Laparoscopic surgery has fewer risks than open surgery and may cause less pain and scarring than open surgery. Laparoscopic surgery also may lead to a faster recovery. Open surgery may be a better option for certain people. If you have a high level of obesity, have had stomach surgery before, or have other complex medical problems, you may need open surgery.*
The type of surgery that may be best to help a person lose weight depends on a number of factors. You should discuss with your doctor what kind of surgery might be best for you.
To read more about the benefits of weight-loss surgery, visit the Weight-control Information Network (WIN) website.
In the United States, surgeons use three types of operations most often: gastric sleeve surgery, also called sleeve gastrectomy, gastric bypass, and laparoscopic adjustable gastric band.
Surgeons use a fourth operation, biliopancreatic diversion with duodenal switch, less often. Each surgery has its own benefits and risks. The patient and provider should work together to select the best option by considering the benefits and risks of each type of surgery. Other factors to consider include the patient’s BMI, eating habits, health conditions related to obesity, and previous stomach surgeries.
Roux-en-Y Gastric Bypass RYGB restricts food intake. RYGB also decreases how food is absorbed. Food intake is limited by a small pouch that is similar in size to the pouch created with AGB. Also, sending food directly from the pouch into the small intestine affects how the digestive tract absorbs food. The food is absorbed differently because the stomach, duodenum, and upper intestine no longer have contact with food.
Vertical Sleeve Gastrectomy | Gastric Sleeve In gastric sleeve surgery, also called vertical sleeve gastrectomy, a surgeon removes most of your stomach, leaving only a banana-shaped section that is closed with staples. Like gastric band surgery, this surgery reduces the amount of food that can fit in your stomach, making you feel full sooner. Taking out part of your stomach may also affect gut hormones or other factors such as gut bacteria that may affect appetite and metabolism. This type of surgery cannot be reversed because some of the stomach is permanently removed.
Laparoscopic Adjustable Gastric Band (AGB) In this type of surgery, the surgeon places a ring with an inner inflatable band around the top of your stomach to create a small pouch. This makes you feel full after eating a small amount of food. The band has a circular balloon inside that is filled with salt solution. The surgeon can adjust the size of the opening from the pouch to the rest of your stomach by injecting or removing the solution through a small device called a port placed under your skin. After surgery, you will need several follow-up visits to adjust the size of the band opening. If the band causes problems or is not helping you lose enough weight, the surgeon may remove it.
Read more from The National Institute of Diabetes and Digestive and Kidney Diseases, Health Information Center.
Examples of possible side effects or complications:
Side effects that may occur later include nutrients being poorly absorbed, especially in patients who do not take their prescribed vitamins and minerals. In some cases, if patients do not address this problem promptly, diseases may occur along with permanent damage to the nervous system. These diseases include pellagra (caused by lack of vitamin B3—niacin), beri beri (caused by lack of vitamin B1—thiamine) and kwashiorkor (caused by lack of protein). Other side effects may include bleeding, infection, leaks from the site where the intestines are sewn together, diarrhea, and blood clots in the legs that can move to the lungs and heart.
Later problems may include strictures (narrowing of the sites where the intestine is joined) and hernias (part of an organ bulging through a weak area of muscle). Two kinds of hernias may occur after a patient has bariatric surgery. An incisional hernia is a weakness that sticks out from the abdominal wall’s connective tissue and may cause a blockage in the bowel. An internal hernia occurs when the small bowel is displaced into pockets in the lining of the abdomen. These pockets occur when the intestines are sewn together. Internal hernias are thought to be more dangerous than incisional ones and need prompt attention to avoid serious problems.
Some patients may also require emotional support to help them through the changes in body image and personal relationships that occur after the surgery.
Read more from The National Institute of Diabetes and Digestive and Kidney Diseases, Health Information Center.